Alcohol Septal Ablation
Definition
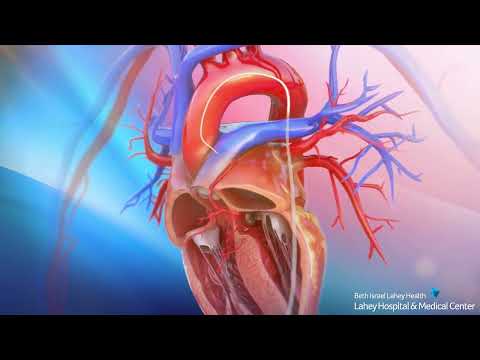
Alcohol septal ablation is a catheter-based procedure that uses alcohol to burn the thickened heart muscle, relieve obstruction, and decrease heart failure symptoms (shortness of breath) in selected HCM patients. Alcohol ablation is performed in the catheterization lab and is an effective alternative for patients who are not candidates for, or do not choose, myectomy surgery.
Procedure
This procedure is performed via a catheter that is first advanced through the femoral artery in the leg up to the coronary artery in the heart. The catheter is positioned in one of the branch arteries supplying blood to the thickened heart muscle. A balloon at the tip of the catheter is inflated. A small amount of absolute alcohol is then injected through the catheter into the heart muscle.
The injection of alcohol causes local injury to the muscle, which triggers a repair process that results in significant thinning of septal muscle thickness. This produces a widening in the heart’s outflow tract which also stops the mitral valve from contacting the ventricular septum.
Patients who come to our HCM Center have access to the most advanced hypertrophic cardiomyopathy treatment options available today. Our Intervention team, including Drs. Thomas C. Piemonte, Gautam Gadey and Arjun R. Majithia, have decades of experience in hemodynamics and alcohol septal ablation.
Results
By eliminating obstruction to blood flow, pressures in the heart are normalized. This results in significant improvement or elimination of heart failure symptoms, similar to surgery.
Alcohol Septal Ablation Procedure for Hypertrophic Cardiomyopathy
Watch our overview of the alcohol septal ablation procedure.